Objectives
After reading this chapter you will be able to:
- describe the roles and responsibilities of program directors
- identify the unique challenges that you may face as a program director
- describe the accountabilities and reporting structures associated with the program director role
- identify the partnerships that are required for program success
- apply practical strategies as you begin your program directorship
- build on the techniques and methods of successful program directors
- describe how you can establish a calendar of ongoing and recurring activities
Introduction
“We would like you to be our next program director.”
These are 10 of the most frightening words one can hear as an educator in medicine. Emotions abound: the desire to do your duty for your program, excitement about providing mentorship and implementing positive change, self-doubt about your candidacy and a sense of helplessness about how to proceed.
Don’t worry. You are not alone. If you have been approached to take on the role of program director (PD), there is a good chance that you are already equipped with many of the requisite skills. As an educator in your program, you are probably involved with resident education and assessment, possibly as a member of the residency program committee (RPC) or competence committee (CC). Transitioning to the PD role is a big step, but it can be one of the most rewarding stages of your career.
Characteristics of a great PD
- Leadership ability
- Ability to negotiate, mediate conflicts, advocate and resolve problems
- Strong communication and interpersonal skills
- Ability to interpret and apply policies and procedures
- Ability to provide effective feedback and familiarity with performance management
- Commitment to continuous learning
Understanding your roles
It is important to reflect on the various roles that will be assigned to you. Each academic institution will have its own job description for program directors, which will outline the qualifications, expectations, resource requirements, duties and responsibilities of the position. Throughout your tenure you will find yourself engaged in all of the roles listed in the job description, even though you may not have had a lot of experience with some of them.
Educational lead
As PD, you will be responsible for the overall administration of the residency program to ensure its success while also making sure that it meets all of the accreditation standards. You will shape the educational landscape of your program by introducing important initiatives to fill curricular gaps to ensure trainees thrive in the learning environment and have a superior educational experience. This will require patience and perseverance as change occurs at the speed of trust1. You will need to partner with other like-minded educators who are willing to support your initiatives or help codevelop new ones. Recognize that not all of your ideas will work; keep trying and don’t get discouraged. The important point is to try to learn from unsuccessful endeavours. The programmatic educational changes you make during your tenure as PD will ultimately be your lasting mark on your program.
Administrator
As PD you will need to work collaboratively with your program administrator (PA) to ensure that your program’s curricular goals are met and monitored. Although your PA is responsible for the administration of your program and one of the most important determinants of your program’s success, be careful not to be passive in your role and leave it solely up to your PA to carry out this duty. Be intentional about how you interact with your PA: schedule regular meetings to review your program together. Additionally, as chair of the RPC, you will be responsible for setting meeting agendas and guiding the processes within your program. Keep your own meticulous records and files. Make time to reflect on your program’s processes; in particular, be on the lookout for situations where these processes are preventing equity, diversity and inclusion (EDI) initiatives from being successful. Be flexible and respectfully challenge them.
Human resources director
During your tenure as PD, you will be responsible for recruiting, selecting and developing your resident group. You are the face of your program, so it is important for you to purposefully reflect on your program’s priorities with your RPC. Recruitment to your program may begin with the first-year medical students at your institution and continue throughout their time in medical school. Every interaction with a medical student is an opportunity to showcase your program and lay the groundwork for attracting the best and brightest to your specialty and program. Your recruitment efforts may also involve critically exploring how your residents’ diversity may or may not reflect the patients they serve.
You will be responsible for meeting with your program’s residents on a regular basis; this will give you a good opportunity to establish a longitudinal relationship that is built on trust and rapport. Through these regular meetings you will provide mentorship and support in addition to carrying out the important task of discussing each individual resident’s progress and learning plans moving forward. Providing residents with honest, constructive feedback on their progress is crucial to their development and growth as a physician in your specialty. Sometimes these conversations can be difficult, especially if a resident is in need of remediation or if there are concerns around professionalism. Seeking guidance from your own mentors, your postgraduate medical education (PGME) office and your department’s human resources personnel can be really helpful. Document these conversations in the resident’s confidential file, for future reference.
Resident advocate
The most important role of a PD is that of resident advocate. It is your duty to ensure that your residents feel safe and supported in their learning environment. Similar to a parent, you must watch over, guide, course correct and, at times, provide tough love to your residents. Securing the support of the residents in your program is crucial to your success. You will be able to achieve this only through listening to their ideas and concerns, which will ultimately build a lasting trust.
The program directorship cycle
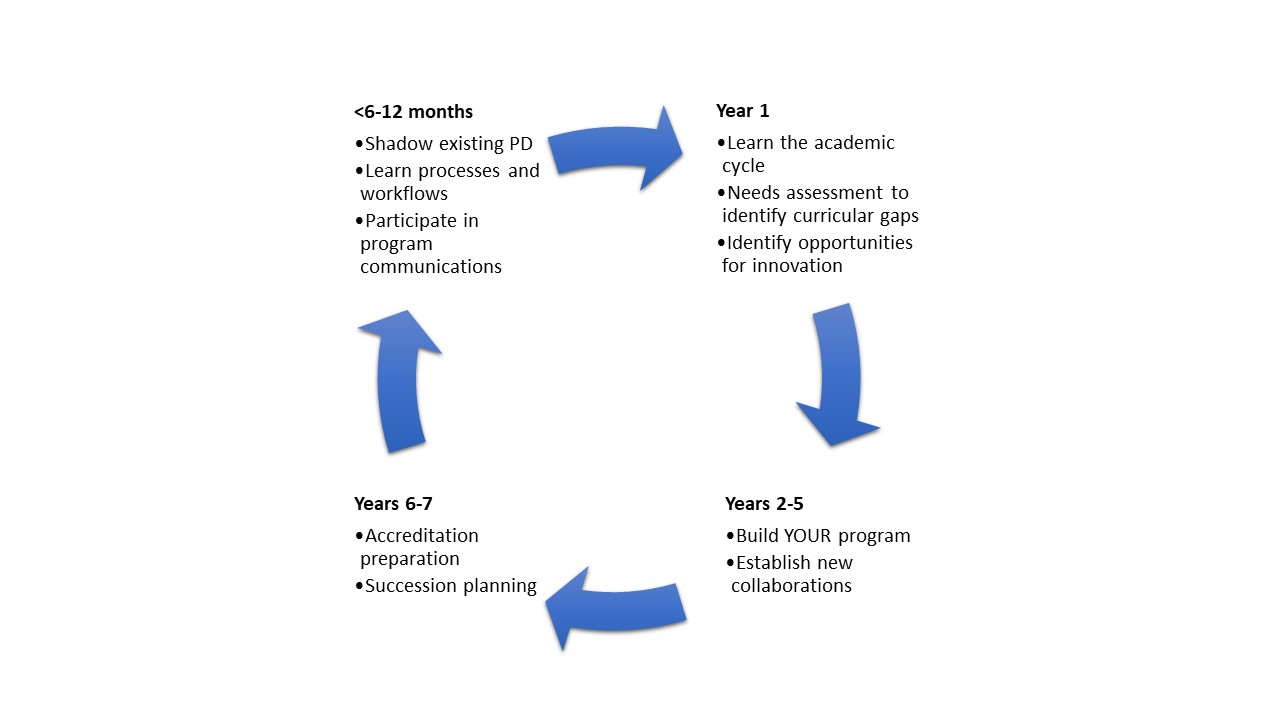
Preparing for your role
Now that you have agreed to become the PD, you will need to familiarize yourself with the day-to-day activities associated with the role. One of the simplest ways to accomplish this is to “virtually shadow” your predecessor, if possible, for six months before your official start date. Arrange to be copied on every email communication that the PD receives and sends. This is an excellent method to start to understand the daily responsibilities of a PD. If this isn’t possible, utilize the time you have and work with your predecessor to design standard operating procedures (SOPs) for the various pieces and processes of the work.
You will have to develop a working knowledge of a variety of sources of documentation at all educational levels, including the national level (Royal College of Physicians and Surgeons of Canada), the university level (your local PGME office) and the program level (documents that are specific to your program). At the national level, The Standards of Accreditation for Residency Programs in Family Medicine (College of Family Physicians of Canada)2 or the Royal College’s discipline-specific standards of accreditation3 are required reading for every PD. These important documents describe the required clinical and academic experiences that will enable residents to obtain the competencies they need, state the expectations of a resident’s performance at the successful completion of training and outline the appropriate structure and organization of a training program.
In addition, you must review and have in-depth knowledge of the CanERA General Standards of Accreditation for Residency Programs,4 which are a national set of standards maintained conjointly by the Royal College, the College of Family Physicians of Canada and the Collège des médecins du Québec, for the evaluation and accreditation of residency programs. These documents serve as the foundation for the assessment and subsequent accreditation of your program. As the incoming PD, it is crucial that you review your program’s last accreditation report to gain a better understanding of the strengths and weaknesses of your program. This will serve as a starting point in the “needs assessment and identification of curricular gaps” in your PD cycle. It is also important to familiarize yourself with Competence by Design5 and CanMEDS.6
Review the important PGME governance policies and procedures at your university. The policy for the assessment of postgraduate trainees is the most crucial, as it sets out the standards for the assessment, promotion, remediation, probation, suspension, extension of training, reintegration and dismissal of trainees in all residency programs. Understanding the principles of trainee assessment will allow you to ensure that there is an appropriate assessment framework that meets the national training standards.
You will also need to learn about the specific tasks required to effectively run your program. A very practical exercise involves reflecting on the yearly academic cycle and making a detailed master schedule of all monthly activities, including all required meetings, examinations and Canadian Resident Matching Service (CaRMS) preparations, as examples. Collaborating with your predecessor in the PD role and your PA will greatly facilitate this activity.
Taking formal training to enhance your preparedness for your new job is highly recommended. For example, each year the Royal College offers a full-day workshop for new PDs. The Royal College extends invitations to the event to all new PDs, typically in their first year. There are also often offerings by local PGME offices for new PDs. To further enhance your communication strategies, instruction in Crucial Conversations7 may be offered by your institution and is an invaluable resource in your PD toolkit. Lastly, many universities, including faculties of medicine, are developing EDI workshops that may help you to bring this lens to your work.
Practical tips for getting started
Assemble your team
Build your team and nurture these relationships. Engagement by every team member is crucial to your program’s success. Having like-minded educators around you in supportive roles is highly recommended as it will provide you with partners with whom you can informally discuss innovation and challenges within your program. At the same time, it is also important to build relationships with educators who have diverse viewpoints or lived experiences to prevent your team from being an echo chamber of the status quo. Developing a strong relationship with your PA is a must. Remember, it takes a village.
Program team members
- Program director
- Assistant program director or other supportive medical education faculty members
- Competence by Design leads — including program, departmental, university (PGME)
- Competence committee chair
- Program administrator
- Residency program committee
- Residents (particularly chief residents)
- Departmental and divisional faculty
- Postgraduate medical education office
Dedicate time and resources
The role of PD requires sacrifice, dedication and time. It is important that you give yourself the opportunity to be successful. Depending on the size of your program, you will need to invest a minimum of a half-day per week in your PD work if your program is smaller and a minimum of one day per week, often more, if your program is larger. This dedicated time enables you to complete your administrative duties, meet with your PA and trainees and spend uninterrupted reflective time on your program. Remember that your time is also a commodity. Appropriate support helps legitimize your role. Review how this support will be provided with your divisional or departmental chair and/or PGME office. Lastly, dedicated PA support is not only crucial to your success but also an accreditation standard.
Tips for academic scheduling
- Send out faculty academic assignments several months before the start of a new academic cycle
- Be sure to send a copy to the administrative assistant of each faculty member
- Have your program administrator send out a weekly reminder to all residents and faculty of the planned activities
- Always look ahead two or three months to prepare for upcoming academic activities
Academic planning
There are many chess pieces to move around the board as you plan out your program, to balance service to your patients and delivery of education. Plan out yearly resident rotations at least six months ahead of the release date. Provide the residents an opportunity for input. Your chief or senior resident(s) can prove to be an invaluable resource to assist you in service scheduling, as can your PA. Be flexible and adaptive to the human resources changes that may occur, often at the last minute. Planning the academic schedule is sometimes a daunting task. Both residents and faculty need to be aware of their academic commitments. By assigning faculty their respective educational responsibilities well in advance, you will minimize cancellations of academic activities. One useful tip is to send to each individual faculty member their complete list of commitments, including specific dates, times and locations, at the beginning of the academic cycle, to provide them the greatest chance of adjusting their clinical responsibilities. Don’t forget to also reach out to faculty who are not members of your program, as they can be excellent resources. Also, be sure to copy each faculty member’s clinical assistant who is responsible for their clinical schedule, whenever you ask for their time. Throughout the year, your PA can send out a weekly reminder of the planned academic activities.
Where to turn for support
- Previous program director
- Program directors from the same specialty at other centres
- Program directors from different specialties at your own centre
- Departmental vice chair, education
- Postgraduate medical education office
- Vice dean or assistant dean
- Royal College of Physicians and Surgeons of Canada
Communication and feedback
It is important to provide educational updates to your residents and faculty on a regular basis. Weekly educational rounds, divisional rounds and journal clubs can be useful avenues for disseminating information. It is equally important for you to receive feedback from all members in your program, especially your residents. By listening to the residents’ concerns, for example through the RPC or an individual conversation, you will enable the program to be responsive to the learners’ needs in a timely fashion. An annual review of the program with residents at an informal venue can be a great team-building exercise and allow the residents the opportunity to provide feedback on the year’s activities while ensuring that the program is undergoing continuous quality improvement. Implementation of an anonymous feedback box, for example, can also provide the residents with a risk-free mechanism to provide program feedback.
Organization
Keep meticulous resident files. Save all programmatic documentation in backed-up electronic files. You will find that this will allow you to continue to build on earlier initiatives and you will be thankful that you have readily accessible information when you need it. Parts of these files may also need to be accessed in an organized way by the competence committee.
Moving forward
As you embark on your program directorship, it is important to remember that although you will be giving yourself over to a unique commitment that will last at least five years, you will be the guiding mentor for a group of residents whom you will steer through their own residency journey. You will make lasting friendships that will be some of the strongest of your career because of the unique bond you will have shared. You will have the opportunity to grow your program and create a lasting culture that will set the foundation for the future.
Inspire your learners and faculty. Most importantly, embrace your role, enjoy yourself and have fun!
Further reading
- Glover Takahashi S, Abbott C, Oswald A, Frank JR. CanMEDS teaching and assessment tools guide. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
- Sherbino J, Frank JR, editors. Educational design: a CanMEDS guide for the health professions. Ottawa: Royal College of Physicians and Surgeons of Canada; 2011.
- Holmboe ES, Durning SJ, Hawkins RE, editors. Practical guide to the evaluation of clinical competence. 2nd ed. Amsterdam: Elsevier; 2018.
- Royal College of Physicians and Surgeons of Canada. Competence by Design for program directors: a practical resource [course]. Available from: www.royalcollege.ca/mssites/cbdpd/en/content/index.html#/
References
- Covey SMR. The speed of trust: the one thing that changes everything. New York (NY): Simon and Schuster; 2008.
- College of Family Physicians of Canada. Standards of accreditation for residency programs in family medicine. Mississauga (ON): College of Family Physicians of Canada; 2020. Available from: www.cfpc.ca/CFPC/media/Resources/Accreditation/2020701-RB-V2-0-ENG.pdf
- Royal College of Physicians and Surgeons of Canada. Directory of primary and subspecialty standards documents. Available from: www.royalcollege.ca/rcsite/ibd-search-e
- CanERA. General standards of accreditation for residency programs. Ottawa (ON): CanERA; 2018. Available from: www.royalcollege.ca/rcsite/documents/canera/general-standards-accreditation-for-residency-programs-e
- Royal College of Physicians and Surgeons of Canada. Competence by Design. The rationale for change. Available from : www.royalcollege.ca/rcsite/cbd/rationale-why-cbd-e
- Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 Physician Competency Framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015. Available from: www.royalcollege.ca/rcsite/canmeds/canmeds-framework-e
- Crucial Learning. Crucial conversations. Available from: https://cruciallearning.com/crucial-conversations-for-dialogue/



