Objectives
After reading this chapter you will be able to:
- describe a practical framework for the implementation of a curricular change using Competence by Design as an exemplar
- identify areas of challenge with the implementation of a new curriculum
- describe key content changes in CanMEDS from 2005 to 2015
Introduction
Although the road to curricular reform may be a daunting one, there are plenty of resources available to make the journey easier. The best tools you have at your disposal are those around you: you are not the first program director (PD) to venture a change in your program. To help you as you embark on this task, we present some lessons learned from our Competence by Design (CBD) journey.
CBD is the Royal College approach to competency-based medical education (CBME), the required curricular reform that respects the uniqueness of the resident’s journey through learning and attaining competence. This novel approach to teaching and assessment utilizing CanMEDS milestones and entrustable professional activities (EPAs) enables regular specific, low-stakes assessments of residents, and more frequent resident review by competence committees, to support resident learning and progression. There are many factors to consider for CBD success that are crucial to resident achievement of competencies and promotion through the stages of training as well as successful program accreditation.
What is required for success in Competence by Design?
- Standardized implementation processes (Royal College, postgraduate medical education [PGME] office)
- Curated resources (Royal College, PGME office)
- Administrative support (PGME office, program)
- Program collaboration, sharing of best practices
- Engaged program director and lead for Competence by Design
- Engaged assessors (residents and faculty)
- Functional ePortfolio with reporting/analytic capabilities
- Engaged and functioning competence committee
Prepare for the change
Assemble and prepare your team
Overhauling your entire program is likely to seem like a daunting task to complete, especially if you try to do so on your own. As you prepare for any curricular reform, especially a big one like CBD, it is important that you assemble a team to work alongside you: identify a lead who has an interest in education; engage those who will be affected by the change (e.g., competence committee members to assist with establishing the structure and function of the competence committee); collaborate with your program administrator; consult with other PDs; and review resources that are provided to you, often by your postgraduate medical education (PGME) office (Figure 6.1).
Preparing for change is everything. Give yourself sufficient time to plan and then to execute on that plan. For a large-scale change such as CBD implementation, start at least 12–24 months before your scheduled launch date. Throughout the change process, continue to power through, even though you may feel like the only cheerleader in your program. It is important to continually engage your faculty in preparing for the change, as their engagement will pave the way for the program’s success.
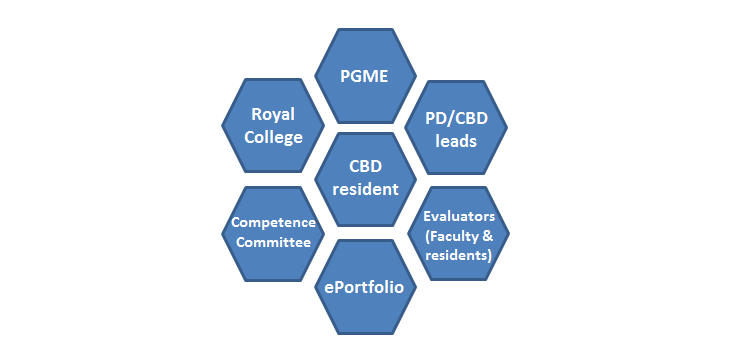
Figure 6.1: Multiple stakeholders will play a role in you program’s curricular change.
Consult your resources
There are often many resources available to help you make curricular changes. Make a point of scanning your usual and not-so-usual sources of support. In our experience, investing the time to find out what already exists should save you a significant amount of effort. For example, the Royal College’s CBD website has an abundance of online resources that can link to theoretical information and hands-on tools. The CBD Resource Directory is a central repository where you can search for specific areas of interest within the topic of CBD, with videos, presentations, handouts, tip sheets and more. The CBD Implementation Planner (found in the Directory) is a useful organizer with checklists for each stage of CBD preparation before launch. Activities in the checklists are grouped into three categories: team and resources, structure, and capacity building.1 Another key resource that the Royal College has developed is Competence by Design (CBD) for Program Directors, a practical, modular-based resource designed to assist PDs with CBD implementation.2
Don’t forget to also explore resources at your institution. For example, to assist local programs, the Office of Education for the Department of Surgery at the University of Ottawa developed a standardized framework for the implementation of CBD. The Competence by Design (CBD) Manual was made available free for download as an Apple Book and proved to be very helpful as we prepared for CBD, in part because it outlines practical key steps for implementation and provides PDs with a playbook and templates for CBD.3
PGME offices at each academic institution will have their own resource library to assist with curricular changes.
uOttawa department of surgery CBD manual
- CBD Readiness
- CBD Structure & Organization
- EPAs & Milestones
- Rotation Planning & Curriculum Mapping
- ePortfolio
- Competence Committee
- Faculty & Resident Development
Develop your faculty
It is important that each program curate their own collection of resources that will aid in their local faculty development. Presentation of such materials at teaching rounds and relevant meetings that have some time dedicated to the upcoming changes will engage your faculty members and get them talking about the changes at hand. Recruitment of educational leads from other programs that have already made similar changes is another great way to hear a different and reinforcing voice. Remember, there’s no reason you have to reinvent the wheel!
Faculty engagement is not a one-time event at the beginning or end of a change. Although faculty development is certainly important early in a change process as a way to socialize an idea, it is also important to have a plan to communicate with faculty and trainees regularly and over time as the change unfolds. Holding sessions on the important pillars of the change is a valuable way to arm faculty with much-needed tools. For example, when implementing CBD, we found CBD 101 workshops, feedback, coaching and the development and distribution of other CBD promotional materials, such as posters, lanyards, and stickers for iPads, assisted program members with EPA recall.
Faculty development topics for Competence by Design
- What are the basics of Competence by Design (CBD), milestones and entrustable professional activities (EPAs)?
- What are your specialty-specific milestones and EPAs?
- What is the faculty’s role in CBD? How will CBD affect clinical workloads?
- What are the residents’ responsibilities in CBD? How does CBD affect resident learning?
- How should you complete an EPA assessment? What makes a good assessment?
- How does bias, such as racism or sexism, show up in assessment? What training is available for faculty to prevent bias?
- How do you access your ePortfolio and navigate an EPA assessment? How do you contact IT for support?
- How should you provide coaching to residents?
- What is the structure and function of your competence committee?
Develop your residents
Resident development is an integral part of any curricular change. It is important to provide adequate onboarding to explain the upcoming change to your residents. Review with them the approach to the curricular change and their roles, responsibilities and expectations. For example, in the context of CBD, it is not sufficient for residents to simply be aware of milestones and EPAs: they are also expected to seek out educational opportunities on a daily basis. There are also expectations around resident self-reflection, and residents are expected to contribute to their own evaluation. Part of your role as the PD is to help residents understand the expectations and develop the skills they need to meet these expectations; this is an important aspect of resident growth. Setting predefined goals for EPA completion assists your residents in stage promotion.
Lastly, if you are implementing a change that may not apply to all residents at the same time or in the same way, be mindful of how the different groups may feel about their inclusion (or lack of inclusion) in the change. In the case of CBD, many program directors were careful not to neglect residents who were in the traditional stream. Although more senior residents’ progression may have been measured against a different (older) set of criteria than that of more junior residents, many PDs made the new curriculum available to their more senior residents for their education. Moreover, the traditional-stream residents were made to feel and see their important role in the change. This was because senior residents ultimately played a formative role as teachers, coaches and evaluators for junior residents and, as such, required instruction so they can partner in the implementation of the curricular change.
Build a framework
To build a framework for major curricular change, like CBD, you will need to create all necessary program documentation, including curriculum maps and new rotation plans, as well as faculty development opportunities. Templates for mapping, planning rotations and other activities are widely available, so make sure to seek out resources that you can leverage — why create something from scratch?
For CBD, for example, the basic tenets of the system are outlined in many documents available on the Royal College website and through your PGME office. Program directors implementing CBD could keep an eye out for tasks that needed to be completed ahead of their CBD launch, as they read through these documents.
Make rotation plans
A curricular change is the perfect time for you and your residency program committee to revisit your current block sequence and reassess the value of all training experiences. It is important to do this well in advance, not only to secure a place for your residents on another service if you are adding an educational experience but also to properly advise the services from which you may be removing residents such that they can adjust. This is a courtesy that could save your PD colleagues trouble around their academic planning. Your university may have specific expectations and guidelines for how to make these changes in an effort to minimize service disruptions. Please ensure you reach out to your PGME office to have discussions about these issues in a timely manner.
Rotation planning and curriculum mapping for Competence by Design: questions to consider
- In which required training experience (rotation) can each entrustable professional activity (EPA) and milestone be obtained?
- Which milestones require formal teaching? How will these milestones be taught?
- Will you need to develop a bootcamp for residents entering the Transition to Discipline (TTD) stage?
- Will you need to tailor rotations to better suit Competence by Design and acquisition of EPAs and milestones?
- Will subspecialty rotations have to be developed for residents to obtain EPAs and milestones?
- Will rotations focused on specific populations (e.g. Indigenous, LGBTQ+) have to be developed to obtain EPAs and milestones? How can you begin to build relationships with providers working in these communities if they don’t already exist?
- Will you need to have first-year residents rotate through their home program in the first 2–3 months to facilitate their acquisition of TTD EPAs and milestones?
- Will you be able to maintain your current academic format?
- Will each EPA have an explicit listing of all milestones on your work-based assessments?
Develop a curriculum map
Developing a curriculum map for the curricular change provides your program with the opportunity to conduct a needs assessment and identify any educational gaps as well as redundancies. Conducting this exercise with your residency program committee or curriculum committee members is highly recommended. Mapping each educational experience (e.g., EPA) to the appropriate clinical rotation will enable your program to reflect on the educational and teaching opportunities that exist for each one and to ensure that each skill can be assessed properly.
Be sure to consider the CanMEDS Roles that are taught and assessed in your program and include these in your curriculum map. In the case of CBD, the Royal College’s EPA Guides in your specialty document suite outline the clinical parameters, assessment plans, relevant milestones and CanMEDS Roles associated with each EPA. Using a master spreadsheet template will facilitate this exercise, and the spreadsheet will serve as a foundation for future accreditation documentation. Examples of such templates are available in CanAMS, the Royal College accreditation management system, or in the University of Ottawa’s CBD manual.3 Templates are also available through local PGME offices and the Royal College’s CBD website. As you go through this exercise, keep in mind the following three questions: What to teach?, How to teach? and How to assess?
Create your infrastructure (including a competence committee)
Make sure that the infrastructure is in place to support your planned curricular change. Be sure to identify what infrastructure and processes are required, what exists already, where there may be gaps and how you will fill those gaps. You may find it helpful to develop standardized templates. For example, in CBD, programs need a competence committee. Although the Royal College has outlined the principles and purpose of the competence committee in a sample terms of reference document,4 the processes and procedures of these meetings are left to the discretion of the program and its CBD implementation team.
Standardized templates are useful for the primary review of resident files by competence committee members before committee meetings and for secondary review, which happens through discussion at the meetings. Likewise, a standardized form is helpful for generating the progress report that is fed to the residency program committee for ratification. The same document can then be shared with the resident. Examples of CC workflow can be found in the University of Ottawa’s CBD manual3 as well as in the Royal College’s online resource Mock Competence Committee Cases for Practical Deliberation.5
Areas for improvement in the implementation of Competence by Design
- Attitudes and existing cultures in programs
- Change management (anxieties, lack of engagement)
- Collaboration between specialties (interuniversity) and programs (intrauniversity)
- Practical knowledge and implementation strategies (Royal College, postgraduate medical education office)
- Administrative support for programs
- IT support for programs
- ePortfolio functionality (reporting and analytic)
- Dependence on multiple electronic platforms for assessments of Competence by Design (CBD) and non-CBD residents
Embrace the change
Large-scale change is usually undertaken in an iterative manner. Major change does not happen overnight. Your program will face new and sometimes unanticipated challenges as the change progresses, and you may feel as though you are struggling to promote your new curriculum. That’s normal. Remember, though, that you are not alone. Even if your change is somewhat unique, many programs have experienced and will experience similar challenges. The people around you, including your colleagues and fellow PDs, are your greatest allies and best resources. By using their tips for success and empowering your team, you will rise to meet the challenges.
Incorporate CanMEDS
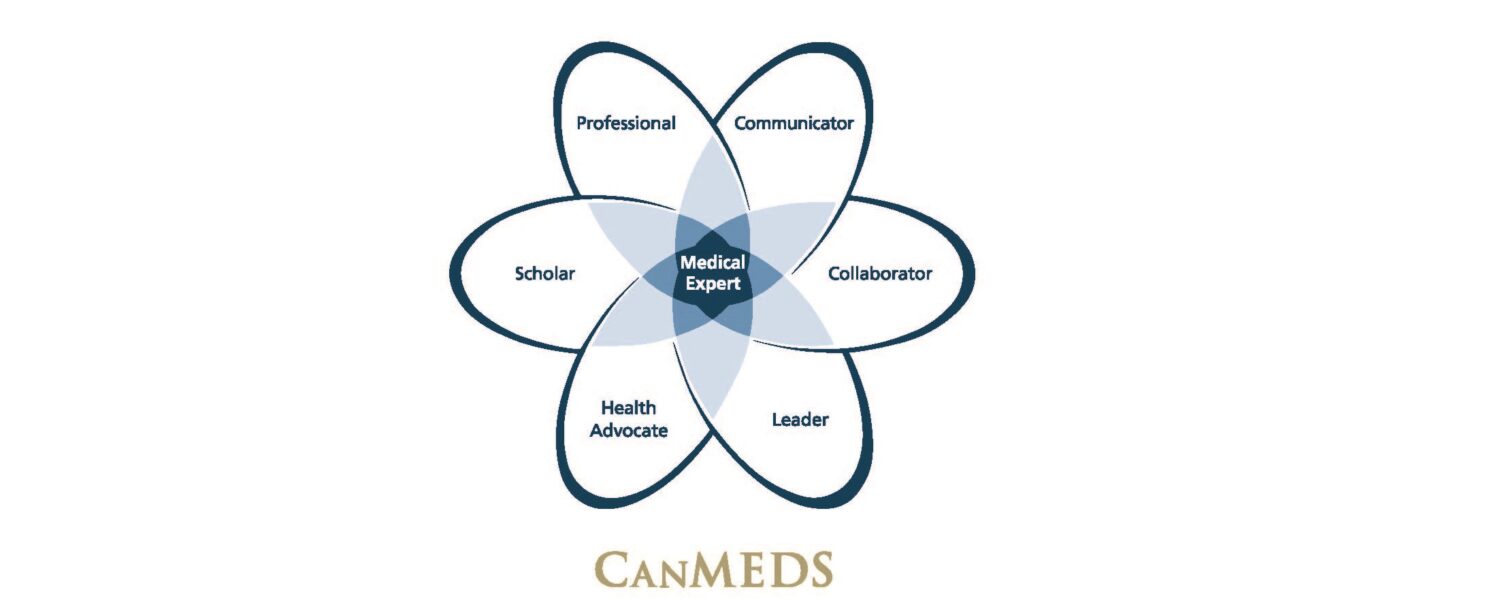
Figure 6.2 CanMEDS Roles
As you know, all programs in Canada must incorporate the competencies of the seven CanMEDS Roles (Figure 6.2) into their curriculum. CanMEDS is the Canadian framework that identifies and describes the abilities that physicians require to effectively meet the health needs of society. The overarching goal of CanMEDS is to have physicians integrate the competencies of the seven roles to improve patient care. The updated version, the CanMEDS 2015 Physician Competency Framework,6 has been integrated into the Royal College’s accreditation standards, CBD, specialty training documents, final in-training evaluations, examination blueprints and the Maintenance of Certification Program. Some of the key content changes from the earlier version include the introduction of new CanMEDS milestones and the inclusion of competencies in safeguarding and enhancing patient safety, quality improvement and resource stewardship.
Design your CanMEDS curriculum
Many of the CanMEDS Roles are implicitly modelled by faculty during clinical activities. Conducting a formal needs assessment of your program will assist you in identifying CanMEDS teaching that already exists in your curriculum and where your educational gaps lie. Regardless of whether the change you’re planning is major or minor, it can be helpful to integrate this needs assessment into the curriculum mapping exercise described above.
Once you have identified your curricular gaps, there are a number of tools and resources that will help you to address these gaps. The Royal College’s CanMEDS Interactive website is a good place to start. The CanMEDS competencies can be filtered according to role and CBD stage to allow for a more comprehensive overview and understanding. Additionally, there is a repository of CanMEDS Role-specific teaching and assessment tools. Further helpful resources and publications are suggested in the accompanying list.7,8 MedEdPORTALis an online journal of teaching and learning resources with many interesting examples of implemented curricula. It is important to use different teaching and assessment strategies to accomplish your curricular goals.
Helpful CanMEDS resources
- Royal College’s CanMEDS Interactive website
- Program materials from past editions of the International Conference on Residency Education
- Royal College’s CanMEDS publications
- MedEdPORTAL
- Postgraduate medical education symposia at your university
- Other programs at your own centre
- Other programs at other centres
Lessons learned…so far
The implementation of a curricular change, like CBD, in your program and understanding how CanMEDS is integrated represent the foundation and framework for your residency training program. To implement any curricular change, whether it is CBD or something else, all faculty will need to be engaged and committed to do their share of the lifting. Invest time in developing your residents and faculty so that they become comfortable navigating the changes and develop a sense of ownership in the new program. Expect challenges along the way, but don’t get discouraged. Learn from those around you and draw upon their experiences.
Best of luck on your journey!
References
- Royal College of Physicians and Surgeons of Canada. CBD implementation planner: for program directors and residency programs. Ottawa: Royal College of Physicians and Surgeons; 2019.
- Royal College of Physicians and Surgeons of Canada. Competence by Design for program directors: a practical resource [electronic course]. Ottawa: Royal College of Physicians and Surgeons of Canada. Available from: www.royalcollege.ca/mssites/cbdpd/en/content/index.html#/
- Watterson JD, Seabrook C, editors. Competence by Design (CBD) manual. Ottawa: Office of Education, Department of Surgery, University of Ottawa; 2019. Available from: https://books.apple.com/ca/book/competence-by-design-cbd-manual-office-education-department/id1472943996
- Royal College of Physicians and Surgeons of Canada. Competence committee guidelines — terms of reference. Ottawa: Royal College of Physicians and Surgeons of Canada; 2018. Available from: www.royalcollege.ca/rcsite/documents/cbd/competence-committees-guidelines-for-terms-of-reference-e
- Royal College of Physicians and Surgeons of Canada. Mock competence committee cases for practical deliberation [electronic activity]. Ottawa: Royal College of Physicians and Surgeons of Canada. Available from: www.royalcollege.ca/mssites/casescenarios_en/story_html5.html
- Frank JR, Snell L, Sherbino J, editors. CanMEDS 2015 physician competency framework. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015. Available from: www.royalcollege.ca/rcsite/documents/canmeds/canmeds-full-framework-e.pdf
- Glover Takahashi S, Abbott C, Oswald A, Frank JR. CanMEDS teaching and assessment tools guide. Ottawa: Royal College of Physicians and Surgeons of Canada; 2015.
- Sherbino J, Frank JR, editors. Educational Design: a CanMEDS guide for the health professions. Ottawa: Royal College of Physicians and Surgeons; 2011.



